
Society loves the idea of bringing children into the world, filling the world with a new generation. However, many fail to think about the women who brings life into the world: mothers. The healthcare field is aware that many women go through postpartum depression but fail to think about how their history greatly impacts this type of depression and how it affects the mother. Healthcare facilities should tailor to every woman’s needs, regardless of prior substance abuse history.
Many people know what postpartum depression is but fail to know how it affects mothers. Postpartum depression (PPD) is “moderate to severe depression in a woman after she has given birth” (Medline) Something that many people do not know is that PPD does not always occur immediately after birth, it can occur up to a year later. Just like a menstrual cycle, pregnancy changes the hormonal leaves in women, leading to changes in mood and increased anxiety. There can be a misconception where people think that a mother can only go into PPD if she has a low income, no family to help, or anything that forces all the parental responsibilities onto the mother. However, well-off mothers with great support from family can experience PPD; it is all about the changes in hormones.
Mothers with previous substance abuse can experience postpartum that is distinctly different from other moms. Substances, such as nicotine, opioids, and cocaine, previously abused by new mothers can increase their risk for PPD. This previous abuse can “limit a mother’s ability to stay emotionally connected to her infant, adjust to his or her rhythms and behaviors, and anticipate or follow his or her development.” (Pajulo 2012) PPD can even cause a mother to relapse, meaning falling back into substance abuse. The road to recovery is a lifetime journey and any major changes to someone’s life can cause a relapse.
The first core issue to discuss is prejudice against women with previous substance abuse history that experience PPD. Doctors can see all medical records for mothers when they come in for checkups after childbirth and their previous history. So, when a mom comes in with concerns about postpartum, the doctors and nurses tending to them already have preconceived notions about them and become timid to help them, in fear that they might abuse any drugs given to them. In turn, moms are forced to go through these troubles alone with no help. “Suicide deaths are a leading cause of maternal mortality in the US. It is a public health crisis that has silently grown worse,” (Admon) As the number of mothers that experience PPD increases, the amount of help and resources decrease.
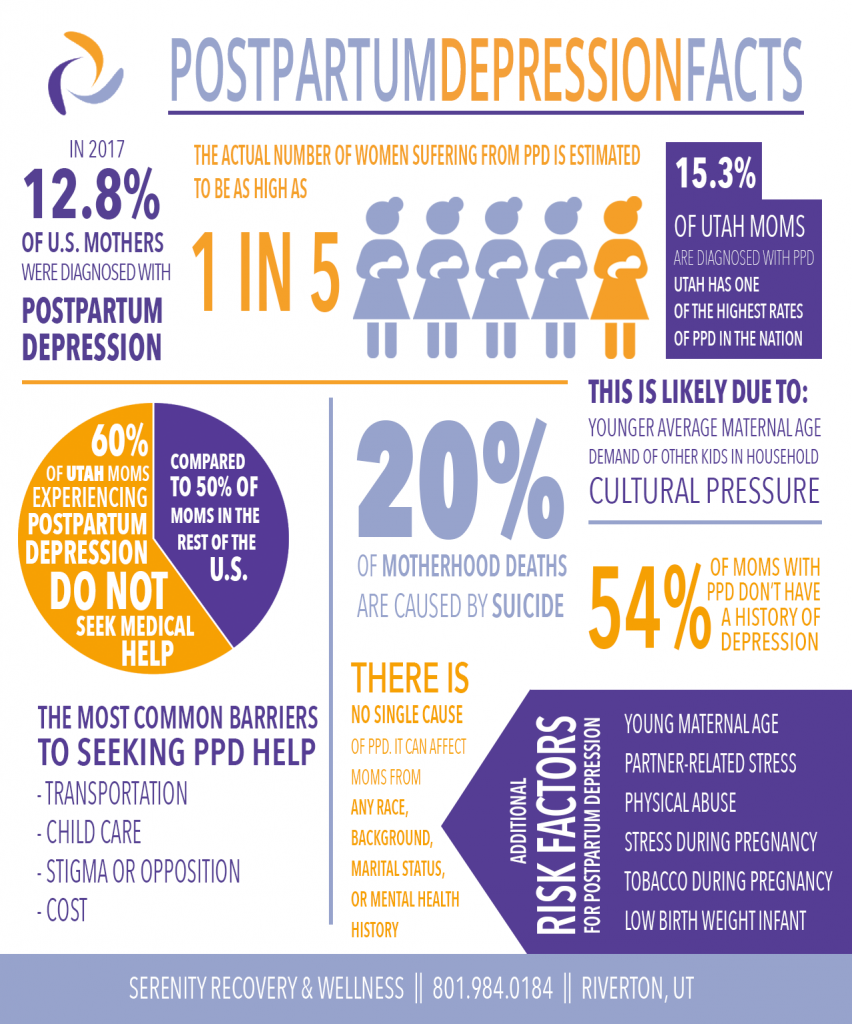
“Nearly 24,000 individuals are at risk for suicide., [making] suicide the leading causes of deaths among new mothers.” (Kuntz 2018) is the statistic that makes this entire article important. This society has women dying, not due to childbirth, but because of the lack of help after. No one truly thinks about the effects that PPD can have on a mother except for a woman who has been through the same troubles. Over time, women have ben losing their voice and settling in their own depression and sadness to make sure that others are okay, leading them to committing suicide. Personally, I have a sister who has prior substance abuse history and had PPD after giving birth to her first child. No one in my immediate family had gone through substance abuse or PPD at the same time. So, we couldn’t understand why she would leave her daughter and not call for days because she was fighting a fight that we had no clue about. Once we realized what was happening, we placed her into an inpatient rehabilitation center, but it did not help because they never got to the real root of the problem which is fighting 2 battles at once. Having PPD and substance abuse history is like fighting World War I and World War II at the same time. Without the right help and a safe zone to talk through your issues, one can fall back into their old ways or give up completely. I want to inform as many people as possible about an issue that goes unnoticed by so many. These women, no matter what they have been through, deserve for their story to be told and we can make changes in the healthcare field to provide guidance to women who do not know what to do next.
As there are more rehab centers being built and are little to no cost for many, there has not been a great change in women-centered facilities. In a study by 3 doctors, all have experience with PPD women, they researched the number of women-centered drug treatment facilities and how much they help women in need of their services. In the centers they studied, they found that the facilities changed little over time in different types of services: “more facilities provided transportation (36% in 2002 vs 38% in 2009) and domestic violence counseling (32% in 2002 vs 36% in 2009), but fewer offered child care (9% in 2002 vs 8% in 2009) and services for pregnant and postpartum women (19% in 2002 vs 15% in 2009).” (Terplan 2015) These small changes indicate a discrepancy in treatment need and service availability to women. Now you may be thinking, “These results are from 2002-2009. There must be many more help centers for these women.” And, sadly, the answer is no. In my own personal research, I searched “women-centered drug treatment facilities” and I only found 1 in my town. Living in the largest city in the United States and there being only one center specifically for women shows the ongoing problem of the lack of women centered facilities who help women fighting PPD and drug abuse. Even with the “Amending Title XIX of the Social Security Act to provide for Medicaid coverage protections for pregnant and postpartum women while receiving inpatient treatment for a substance use disorder, and for other purposes” (Walden 2018) it is still difficult to find facilities that help women with both PPD and drug abuse and also provide them with the certain circumstances that they need, such as childcare and transportation. As a society who likes to take measures into their own hands, what can we do?
As we look toward solving this ongoing problem, doctor’s and specialists must change previous timespan checkups to oversee these women for longer periods of time and develop new facilities that assist women with a substance abuse background and provide them with the help and support they need. One solution that can implemented by the healthcare field is increasing the number of checkups on mothers after childbirth. On average, mothers receive checkups “two to three weeks postpartum and then again at six to eight weeks postpartum” to check up on their health after childbirth. (TheBump) During these checkups, most doctors just check your blood pressure, vitals, and belly to ensure that everything is healing good physically. According to Baby Center, the purpose of a 6-week checkup is “to check on your physical recovery from pregnancy and delivery, see how you’re doing emotionally, and address your needs going forward.” (Baby Center) With these being the only checkups for the mothers, doctors fail to check on the mental state of these women. Healthcare workers should be looking at all aspects of a human’s state of needs: physical state, emotional state, and mental state. So far, women are receiving help for the physical state, while their mental state is being disregarded. Being that all mothers are different, I think that there should be a coordinator for all mothers where they implement a set of dates that extends specialized maternal care that works for each specific woman’s needs. With this new plan, mothers can receive checkups for their mental and emotional state of being.
Another solution that can be fulfilled by government or future business owners to open new facilities that actively support PPD women with precious substance abuse. There are hotlines, such as SAMHSA’s National Helpline, who help individuals and families facing drug abuse problems and any mental disorders by proving them with information about local treatment groups and community-based organizations. (SAMHSA) However, as I want to be a business owner in the future, I plan on opening a women-center facility called “Mommies in Need” who help new moms with possible PPD symptoms, moms facing PPD currently, moms with prior drug abuse, and so much more. I will work to provide support groups, online and in-person, for any mom or families who need someone to talk to and possibly find someone to relate with or talk to more after the program. I would also provide other services such as childcare for women who cannot find someone to watch their children while attending these services and computers for women who need more help beyond just drug abuse and PPD. Lastly, this program does not have a set start date or end date. Women are allowed to come back whenever they need help because anything can trigger depression or drug abuse at any stage of the healing process. As a society, we must move away from having a specific time and date on everything because we are all humans, but we are all different.
In conclusion, women fighting PPD and prior drug abuse can be looked down upon so much and ignored about any problems they face after childbirth. As more children are being brought into the world, the less the number of women-centered rehab centers work to help new moms. Instead of pushing away PPD women with drug abuse and setting specific times on the healing process, we should construct plans specific to each mother after childbirth and open new businesses that aid mothers in getting the help that they most certainly deserve. Motherhood is hard and no one knows that better than a mama.

Reference List
Kuntz, Leah. https://www.psychiatrictimes.com/view/pregnancy-and-postpartum-suicide-risk-the-new-numbers. Nov 2020.
Amending Title XIX Of the Social Security Act to Provide for Medicaid Coverage Protections for Pregnant and Postpartum Women While Receiving Inpatient Treatment for a Substance Use Disorder, and for Other Purposes : Report (to Accompany H.R. 5789) (including Cost Estimate of the Congressional Budget Office). [U.S. Government Publishing Office], 2018.
Terplan, Mishka, et al. “Women-Centered Drug Treatment Services and Need in the United States, 2002-2009.” American Journal of Public Health (1971), vol. 105, no. 11, American Public Health Association, 2015, pp. e50–e54, https://doi.org/10.2105/AJPH.2015.302821.
Kuo, Caroline, et al. “A Qualitative Study of Treatment Needs Among Pregnant and Postpartum Women with Substance Use and Depression.” Substance Use & Misuse, vol. 48, no. 14, Informa Healthcare, 2013, pp. 1498–508, https://doi.org/10.3109/10826084.2013.800116.
SAMHSA. SAMHSA’s National Helpline. https://www.samhsa.gov/find-help/national-helpline. 2022
Aggarwal, Nheal https://www.thebump.com/a/postpartum-checkup 2021.
Martin, Caitlin E, and Anna Beth Parlier-Ahmad. “Addiction treatment in the postpartum period: an opportunity for evidence-based personalized medicine.” International review of psychiatry (Abingdon, England) vol. 33,6 (2021): 579-590. doi:10.1080/09540261.2021.1898349
Leave a Reply